Gabapentin is used with other medications to prevent and control seizures. It is also used to relieve nerve pain following shingles (a painful rash due to herpes zoster infection) in adults. Gabapentin is known as an anticonvulsant or antiepileptic drug.

Gabapentin, also known by the brand name Neurontin, is a prescription painkiller belonging to its own drug class, Gabapentinoids. It is considered an anti-convulsant, and is most commonly used to treat epilepsy, restless leg syndrome, hot flashes, and neuropathic pain. It is often used as a less-addictive alternative to opioids; however, Gabapentin addiction and abuse still occur in many patients.

Gabapentin has a similar chemical structure to Gamma-aminobutyric acid (GABA), the brain chemical which affects the body’s nervous system. It can produce feelings of relaxation and calmness, which can help with nerve pain, anxiety, and even poor sleep.
Gabapentin is prescribed to treat nerve pain, alcohol and cocaine withdrawals, restless leg syndrome, diabetic neuropathy, fibromyalgia, and seizures. It works by altering one’s calcium channels to reduce seizures and ease nerve pain. Some brand names of Gabapentin are Neurontin and Gralise. The drug’s known street names are “gabbies” or “johnnies.”
Dosages of Gabapentin

Adult and pediatric dosages:
Capsule

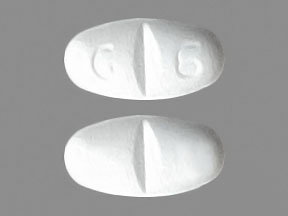
Tablet
-
-
- 300 mg (Gralise)
- 600 mg (Gralise, Neurontin)
- 800 mg (Neurontin)
Dosage Considerations – Should be Given as Follows:
Reducing the dose, discontinuing the drug, or substituting an alternative medication should be done gradually over a minimum of 1 week or longer.
Geritric dosing considerations:
Renal impairment is present, gabapentin dose reduction may be required, depending on renal function.
Partial Seizures
Neurontin
Adjunctive therapy for partial seizures with or without secondary generalization.
Initial: 300 mg orally every 8 hours.
May increase up to 600 mg orally every 8 hours; up to 2400 mg/day administered and tolerated in clinical studies; up to 3600 mg administered for short duration and tolerated
Post herpetic Neuralgia
Neurontin
Day 1: 300 mg orally once per day.
Day 2: 300 mg orally every 12 hours.
Day 3: 300 mg orally every 8 hours.
Maintenance: Subsequently titrate as needed up to 600 mg orally every 8 hours; doses greater than 1800 mg/day have demonstrated no additional benefit.
Gralise
Dose gradually to 1800 mg/day orally; take once a day with evening meal.
Day 1: 300 mg orally once a day.
Day 2: 600 mg orally once a day.
Days 3-6: 900 mg orally once a day.
Days 7-10: 1200 mg orally once a day.
Days 11-14: 1500 mg orally once a day.
Day 15 and after (maintenance): 1800 mg orally once a day.
Dosing considerations:
Gralise tablets swell in gastric fluid and gradually release gabapentin. Swallow Gralise tablets whole; do not cut, crush, or chew them.
Dosing Modifications:
Renal impairment (Neurontin)
Creatinine clearance greater than 60 mL/min: 300-1200 mg orally twice daily
Creatinine clearance 30-60 mL/min: 200-700 mg every 12 hours
Creatinine clearance 15-29 mL/min: 200-700 mg once per day
Creatinine clearance less than 15 mL/min: 100-300 mg once per day
Hemodialysis (Creatinine clearance less than 15 mL/min):
Administer supplemental dose (range 125-350 mg) post hemodialysis, after each 4 hour dialysis interval; further dose reduction should be in proportion to Creatinine clearance (a Creatinine clearance of 7.5 mL/min should receive one-half daily post hemodialysis dose)
Renal impairment (Gralise):
Creatinine clearance is greater than or equal to 60 mL/min: 1800 mg daily with evening meal
Creatinine clearance 30-59 mL/min: 600-1800 mg daily with evening meal
Creatinine clearance greater than 30 mL/min or hemodialysis: Do not administer
In addition its potentially addictive nature, Gabapentin can cause suicidal thoughts, moods swings, and abrupt changes in a user’s behavior. It can also cause elevated blood pressure, fever, sleep problems, appetite changes, and chest pain.
Gabapentin may cause side effects. Tell your doctor if any of these symptoms are severe or do not go away:
-
-
- drowsiness
- tiredness or weakness
- dizziness
- headache
- uncontrollable shaking of a part of your body
- double or blurred vision
- unsteadiness
- anxiety
- memory problems
- strange or unusual thoughts
- unwanted eye movements
- nausea
- vomiting
- heartburn
- diarrhea
- dry mouth
- constipation
- increased appetite
- weight gain
- swelling of the hands, feet, ankles, or lower legs
- back or joint pain
- fever
- runny nose, sneezing, cough, sore throat, or flu-like symptoms
- ear pain
- red, itchy eyes (sometimes with swelling or discharge)
Some side effects may be serious. If you experience any of the following symptoms, call your doctor immediately:
-
-
- rash
- itching
- swelling of the face, throat, tongue, lips, or eyes
- hoarseness
- difficulty swallowing or breathing
- seizures
- difficulty breathing; bluish-tinged skin, lips, or fingernails; confusion; or extreme sleepiness
Gabapentin may cause other side effects. Call your doctor if you have any unusual problems while taking this medication.
If you experience a serious side effect, you or your doctor may send a report to the Food and Drug Administration’s (FDA) MedWatch Adverse Event Reporting program online (http://www.fda.gov/Safety/MedWatch) or by phone (1-800-332-1088).
Gabapentin Abuse
Gabapentin abuse tends to occur in people who already have an addiction to opioids or other drugs. The effects of Gabapentin intoxication have been described as a sense of calm, euphoria, and a high similar to marijuana.
A 2013 study in Kentucky found that of the 503 participants reporting illegal drug use, 15% reported using Gabapentin in addition to other drugs to get high in the previous six months. Another study, working with a sample of participants meant to represent the national population, found almost a quarter of patients with co-prescriptions of opioids and Gabapentin were getting more than three times their prescribed amount to supply their addiction. People using the drug without a prescription is a growing problem in many areas. Due to the drug’s legal status, this is difficult to address from a policing standpoint. States where Gabapentin abuse is becoming more common are beginning to classify the drug as a more strictly controlled substance.
Signs of a Gabapentin Overdose
Effects of excessive Gabapentin use include:
-
-
- Drowsiness
- Coordination problems
- Tremors
- Dizziness
- Depression
- Suicidal thoughts/behaviors
- Changes in mood
- Dizziness
- Poor coordination
- Forgetfulness
- Anxiety
- Difficulty speaking
- Inability to feel pleasure
It is important to try to recognize these symptoms and to be wary of other red flags, such as the presence or abundance of pill bottles. These effects can be detrimental to one’s health, livelihood, and overall safety.
Many Gabapentin users in early recovery abuse Gabapentin because at high doses (800mg or more), they may experience a euphoric-like high that does not show up on drug screens. Gabapentin abusers typically take the drug in addition to opioids to produce their desired high, a dangerous and potentially deadly combination. It is possible to fatally overdose on Gabapentin, both on its own or in conjunction with other drugs. However, there is currently no antidote that can be administered to someone in the case of a Gabapentin overdose as there is with opioid overdoses. If you find a loved one showing signs of an overdose–drowsiness, muscle weakness, lethargy and drooping eyelids, diarrhea, and sedation—seek medical attention immediately.
Signs of Gabapentin Addiction
-
-
- Lying about or exaggerating symptoms to doctors
- Seeking out multiple doctors to get extra doses
- Switching doctors after the original doctor refuses to continue prescribing the medication
- Changes in social habits and/or circles
- Changes in personal hygiene and grooming habits
- Constant preoccupation with the drug
- Unease at the thought of the drug being unavailable
- Refusal to quit despite social, financial, or legal consequences
- Failed attempts to quit
Treating a Gabapentin Addiction

Frequent and excessive use of Gabapentin can lead to a physical and psychological dependence on the drug. This is when someone becomes so accustomed to taking a drug that they need it to feel and function normally. Quitting a drug like Gabapentin cold turkey can be dangerous and induce several withdrawal symptoms of varying severity.
These include anxiety, insomnia, nausea, pain, and sweating. Quitting also increases one’s likelihood of having a seizure which can lead to personal injury or the development of medical problems and life-threatening emergencies. Trying to quit should be done at a rehab facility or with the guidance and supervision of a professional during a medical detox.